- HOME
- Staff of Doctors
- Health Centers
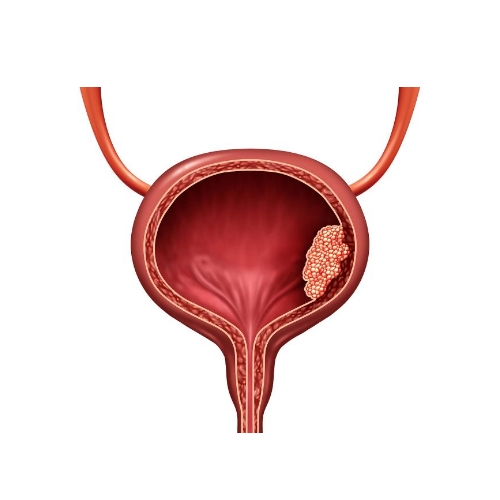
- Health Service
HEALTH CENTERS of HAPPY GREEN LIFE
- Beauty Services
DENTAL BEAUTY BODY SCULPING RHINOPLASTY HAIR TRANSPLANT
- Blog
- TourismIRAN`s NATURE ATTRACTIONIran is a country blessed with a diverse range of natural attractions, including impressive.IRAN`s NATURE ATTRACTIONHISTORICAL REGIONS OF IRANIran has had many historical regions over time, each with its own unique culture and history. Some of the most significant regions...Tourism in IranIran is a country blessed with a diverse range of natural attractions, including impressive mountain ranges, vast deserts, lush forests, and stunning coastal areas...

DIVING
Diving With our expert leaders in IRAN

Mountain

ski

shoping

Fishing

Horse Riding
In beautiful places like no where.

Photography
- Certificates
English
- HOME
- Staff of Doctors
- Health Centers
- Health Service
HEALTH CENTERS of HAPPY GREEN LIFE
- Beauty Services
DENTAL BEAUTY BODY SCULPING RHINOPLASTY HAIR TRANSPLANT
- Blog
- TourismIRAN`s NATURE ATTRACTIONIran is a country blessed with a diverse range of natural attractions, including impressive.IRAN`s NATURE ATTRACTIONHISTORICAL REGIONS OF IRANIran has had many historical regions over time, each with its own unique culture and history. Some of the most significant regions...Tourism in IranIran is a country blessed with a diverse range of natural attractions, including impressive mountain ranges, vast deserts, lush forests, and stunning coastal areas...

DIVING
Diving With our expert leaders in IRAN

Mountain

ski

shoping

Fishing

Horse Riding
In beautiful places like no where.

Photography
- Certificates
English